Introduction of Taiwan Health Center

In 2007, the Republic of China (Taiwan) government established the Taiwan Health Center in the Republic of the Marshall Islands (RMI). The purpose is to provide medical care and public health education for the Marshallese people.
Taipei Medical University Shuang-Ho Hospital and the Ministryof Health and Welfare (Taiwan) undertook the project of TaiwanHealth Center in 2013. We developed many healthcare programsin accordance with the major health issues of the Marshallesepopulation. Under the supervision of the Republic of China (Taiwan)Embassy in the Republic of the Marshall Islands, Taiwan Health Centercooperates with various local medical institutions in order to promotepublic health in the Marshall Islands.
Over the past few years, the Taiwan Health Center has performed many medical projects. Now, we are going to introduce some of the projects we have done in recent years.
 |
 |
DM Community Screening Project
According to the WHO statistics, the prevalence of diabetes in the Marshall Islands is one of the highest countries in the world. Diabetes-related diseases have been the main cause of death among all Marshallese. Therefore, since 2015, Taiwan Health Center has been cooperating with the Ministry of Health of Marshall Islands and the Canvasback Wellness Center to provide a Community Lifestyle Program (CLP) in several communities. Furthermore, we also launched a two-week program of diabetes seed-teacher training in Laura. The activities include diabetes screening, hypertension screening, diabetic foot examination, doing exercise, cooking demonstration and health education.
In each community, we referred people with newly diagnosed diabetes or poor glycemic control to the hospital for further intervention. In order to make sure they come to the hospital, we cooperated with the public health nurses to remind every referred patient comes back to the clinic by phone alert. Through these activities, we hope that we can have some positive effects on the lifestyle of the Marshallese people and decrease the prevalence of Diabetes in the Marshall Islands.
Community Lifestyle Program (CLP)
 |
 |
|
 |
 |
NCD Clinic and NCD out-reach
Since 2016, Shuang-Ho Hospital sent two physicians to the RMI to assist the public health program of Taiwan Health Center. During their stay, the two physicians assisted None- Communicable Disease (NCD) clinic and provided healthcare for over 1000 patients with Diabetes in Majuro Hospital. In addition, they participated in the weekly home visits of the public health sector to treat patients with disabilities or financial problems. The physicians went inside every patient’s home to perform healthcare and provide medication. Through the NCD clinic and the out-reach project, Taiwan Health Center has delivered the medical services to the people in great need.
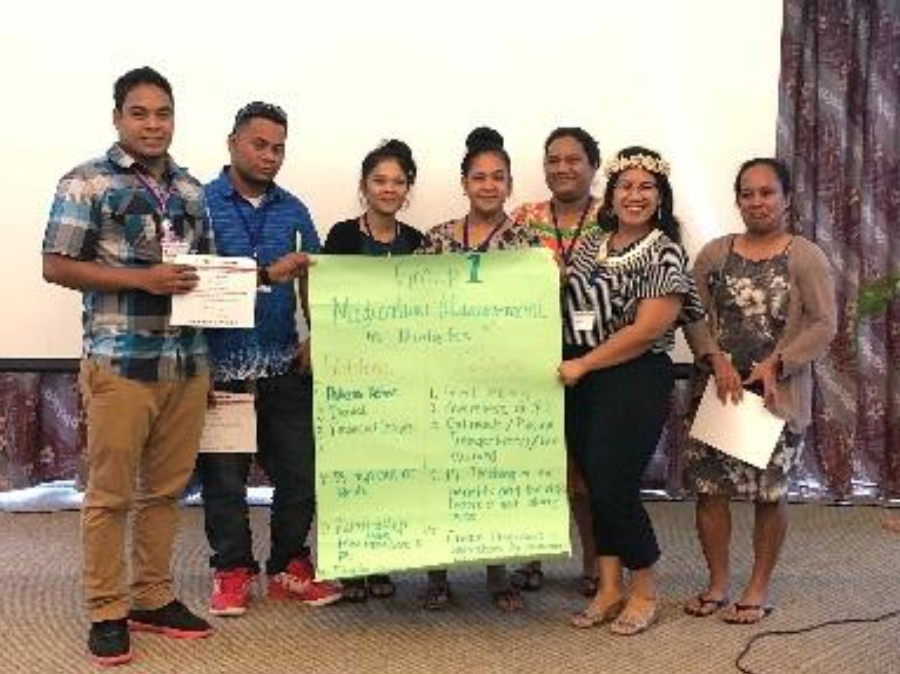
Non-Communicable Disease Conference
Taiwan Health Center has developed an outstanding relationship with Ministry of Heath of RMI and many local non-governmental organizations. We have been able to cooperate and integrate our resources to bring the freshest knowledge and information about health to the healthcare provider of RMI. In every October, a Non- Communicable Disease International seminar is held. In recent years, the number of the participants has hit record highs. Our speakers were the professional experts in different fields from Taiwan as well as from other countries. Taiwan Health Center was very willing to provide resources for the people of the RMI through these seminars. We hope that we can inspire Marshallese people to pursuit a healthy lifestyle, and support them to win the battle against NCD.
 |
 |
 |
Short-term Medical Mission
Every year, Taiwan Health Center sends physicians with different specialty to provide medical services for the people of RMI. Responding to the lack of medical resources in the Marshall Islands, the physicians have increased their length of stay in the RMI from two weeks to a month. Every year, Shuang-Ho Hospital has dispatched at least 8 short- term physicians including cardiologists, ENT physicians, dermatologist, Pediatrics metabolic physician and pulmonary physician, the dispatched specialists not only perform regular outpatient duties but also work with Medical Internship Training Program. The extension of the stay allows the physicians to be more integrated into the Marshallese local health care system so that they can provide more comprehensive care. The health professionals provided medical care for the Marshallese citizens have received praise for their hard work. Taiwan Health Center is honored to provide the medical services here, and looks forward to extending more supports in the near future.
Medical Training of Chronic Disease
Continuing education is necessary for every healthcare provider. Therefore, Taiwan Health Center held medical training of Diabetes and Hypertension to provide more comprehensive viewpoint for the medical staffs in the Marshall Islands. During the workshop, we shared the up-to-date medical information and exchange the knowledge with the healthcare provider. We received many positive feedbacks. Therefore, we will continue to hold the event in the Marshall Islands in the future.
 |
 |
 |
PACS and Medication Donation
The infrastructure of the hospital stands an important role in the quality of medical care. Under the fully support from the Republic of China (Taiwan) Embassy in the Republic of the Marshall Islands, Taiwan Health Center has helped Majuro Hospital enhance the quality of medical care by donating the Picture Archiving and Communication System (PACS) and fingerprint system. The systems simplify the process of images reading, facilitate the keeping of medical records and elevate the level of medical care in Majuro Hospital. It is the cornerstone of the support in the infrastructure from Taiwan Health Center to Majuro Hospital. In the near future, we build a customized Hospital Information Systems (HIS) in the Majuro Hospital, hoping it can bring a promising future of medical services to the people of RMI. Apart from helping to build the information system, Shuang Ho hospital donated medical supplies at the very first moment to the Marshall Islands when there was a outbreak. This act showed that Taiwan Health Center is always on the same side with the Marshall Islands, deeply concerning about the Marshallese people.
 |
 |
 |

